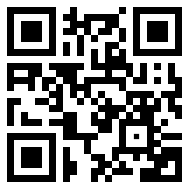
Medical Alert Information
Please read before treating me.

I have a rare metabolic condition called Pompe Disease. This is a type of Muscular Dystrophy that limits my ability to breathe unaided, if led down or reclined too far, and move with difficulty.
Serious risk of death by respiratory failure when reclined or led flat
Personal Details
D.O.B: 15/03/1962
NHS No: 486 567 1188
Next of Kin: Liz Foxwell – Wife
Liz’s mobile: 07824 612 965
Mobile unlock code: 150362
DNR: I have a DNR in place, a copy is on my phone
Conditions: Pompe Disease and Type 2 diabetes
Bleeding: I am on 2.5mg of Apixaban, blood thinners
Medication: Dulaglutide, Ramipril, Mirtazapine, Apixaban
Metabolic Consultant: Dr Duncan Cole – Cardiff University Hospital, 029 21 843 403
Respiratory Consultant: Dr Fairbairn, St Woolos Hospital
Respiratory Nurse: Amy
Neurology Consultant: Dr Ken Dawson, Nevill Hall Hospital
Diabetic Consultant: Professor Peter Evans
Consultant Ophthalmologist: Dr Rita Singupta
Do not lie me flat or I will die.
I cannot breathe unaided when led down or reclined. I need a BIPAP machine which is a non-invasive ventilator otherwise I will die or suffer oxygen starvation within minutes.
I have a BIPAP ventilator in the boot of the car and by the side of my bed.
Difficulty Rising
My muscles are weak and I cannot rise from the ground without assistance. Please help me sit up as soon as possible.
High Flow Oxygen will shut down my breathing
Do not give oxygen before checking end tidal or blood C02 levels. A low oxyhaemoglobin saturation may indicate C02 retention and need positive pressure ventilation. If supplemental oxygen is given continuously monitor C02 levels. Non invasive bi-level ventilation will be required.
Mechanical cough assist will be needed to clear mucus.
Respiratory Care Information
Normal Partial Pressure of Carbon Dioxide (PC02) and End Tidal Carbon Dioxide (CO2): 35-45 mmHg – Normal Oxygen Saturauion (Sa02): 95 – 100%
Pompe Symptoms
The symptoms of Late Onset Pompe Disease (LOPD) are listed below.
People with LOPD may have some or all of the symptoms below.
Head and Shoulders
- Muscle weakness in eyes
- Dropped eye lids
- Morning headaches
- Sleep apnoea
- Uses a BiPAP to breathe
- Difficulty swallowing
- Difficulty clearing airway after eating
- Weak cough
- Difficulty clearing throat
- Speaking voice changed, volume, texture
- Impaired alertness
Arms and hands
- Weak grip
- Struggling to hold items
- Arms feeling heavy
- Difficulty lifting arms above shoulders
Body/Torso
- Protruding stomach
- Bowel issues
- Bladder frequency/leakage
- Respiratory insufficiency/failure
- Muscle weakness in mid section
- Difficulty bending and straightening
- Continence Issues
Hips and Legs
- Difficulty getting up from a seated position
- Difficulty bending and straightening Difficulty climbing stairs
- Weaker front thigh muscles Unsteady when standing for longer periods
- Waddling gait
- Unable to stand alone
- Muscle cramps
- Struggling to walk
- Thicker calf muscles
- Tightness in calf muscles
- Pain when standing for short/long periods
- Unsteadiness when turning round
- Difficulty lifting foot
- Dropped foot, sometimes feels heavy/sags
Some users are reliant on a wheelchair or walking aid
General Well Being
- Feeling tired
- Temperature regulation – feeling hot/cold
- Tremors – feeling shaky
- Limbs feeling heavy
- Feeling totally exhausted
- Mental health – depression/anxiety
Test Results (may show anomalies in the following)
- Low oxygen levels
- Raised CO2 levels
- Raised Creatine kinase (CK) levels
Please be aware that the person may be on Enzyme Replacement Therapy (ERT).
Addition Support and Therapies
This person will also have a metabolic consultant that should be consulted prior to treatment and/or therapies.
- Enzyme Replacement Therapy
- Dietitian – High protein, low carb, low sugar
- Physiotherapist – 70% sub maximal
- Counselling – Mental Health
- Respiratory Consultant